What is Plaquenil or hydroxychloroquine?
Hydroxychoroquine is an oral medication used for the treatment of rheumatologic conditions like lupus (systemic lupus erythematosus – SLE), rheumatoid arthritis and other inflammatory conditions. It is generally a safe medication however chronic use or too high of a dose of chloroquine (CQ) and hydroxychloroquine (HCQ) can cause retinal toxicity.
What does Plaquenil/hydroxychloroquine do to your eyes?
The retina is the film in the back of your eyes. CQ and HCQ can both cause maculopathy or retinopathy. Prior to modern diagnostic techniques, your eye doctor was looking for bull’s eye maculopathy with a dilated exam. With today’s high technology approach, we hope to never see bull’s eye maculopathy again but rather prevent toxicity at an earlier stage before it affects your vision. Once toxicity occurs, it is irreversible and can continue to progress for a short time even after stopping the medication. The toxicity appears to be more central in non-Asians and more along the arcades in Asian patients.
The American Academy of Ophthalmology (AAO) recently put out an updated statement on the medical recommendations for screening for toxicity in March 2016.
What are the risk factors for toxicity?
The main risk factor is the dose as well as the duration of therapy. The updated guidelines recommend a maximum daily dose of HCQ of ≤ 5.0 mg/kg real weight and ≤ 2.3 mg/kg/day of CQ. Doses upto 20 mg/kg/day showed 25-40% risk of retinopathy. At the recommended dose, the risk of toxicity is low at <1% in the first five years of therapy and <2% upto 10 years. Figure 4 and 5 (in AAO statement) demonstrate the risk with duration and dose of therapy.
Additional risk factors for toxicity include: renal/kidney disease, concomitant tamoxifen use (drug used in breast cancer) with a 5-fold increased risk and a previous retinal or macular disease which can make monitoring for toxicity more difficult for your eye doctor. HCQ is metabolized by the cytochrome P450 enzymes and can have cross-reactivity and increase toxicity when taken with other drugs metabolized via the same pathway.
What are the recommendations for screening?
A baseline dilated eye exam by an experienced ophthalmologist as well as visual fields and SD-OCT looking for contraindications for therapy such as pre-existing macular changes. Thereafter, the AAO states annual screening can be deferred until year 5 on the medication but should start sooner if the patient is at a higher risk for toxicity.
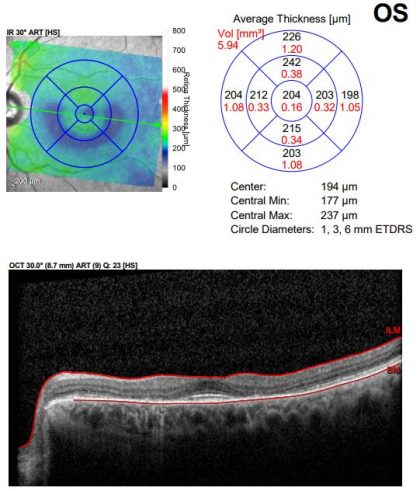
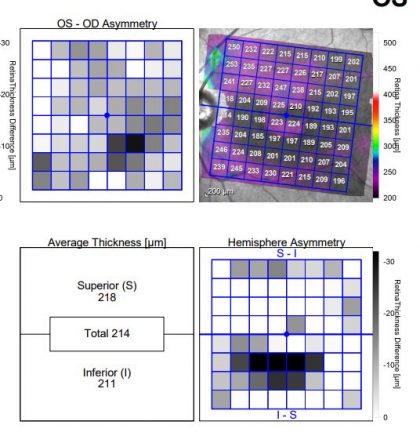
The guidelines recommend 1) an automated visual field as well as a 2) spectral-domain optical coherence tomography (SD OCT). Other tests can include fundus photos with auto-fluorescence (FAF) and multifocal electroretinogram (mfERG) but the latter requires skilled technicians to perform the test well.
What does toxicity look like?
Toxicity causes a parafoveal or extramacular loss of photoreceptors and the retinal pigment epithelium layer (RPE). End stage maculopathy causes a bull’s eye pattern of RPE loss as well as possible cystoid macular edema, loss of central and peripheral vision as well as night vision. Refer to the AAO’s statement link for photos of toxicity as well as below.
Are there supplements I can take to prevent maculopathy?
The major macular disease which we know more about is age-related macular degeneration (ARMD) for which the NIH has guideline to help protect the macula including oral supplements of lutein and zeaxanthin. It is not known whether this would benefit patients on HCQ or those with toxicity.
Photos of one of Dr. Pradhan’s patients (not on HCQ for years now):
As you can see, the fundus photo is a subtle finding, however the toxicity shows up well on the OCT multi-color photo. The OCT also reveals the permanent bull’s eye pattern of RPE loss.